Page 94 - Combine
P. 94
International Journal of Trend in Scientific Research and Development (IJTSRD) @ www.ijtsrd.com eISSN: 2456-6470
The present study showed that AMI is diagnosed only in 40% of patients with elevated troponin-T without a typical clinical
picture of AMI. The remaining patients had another underlying disease with manifestations of multiple organ failure. It should
be emphasized that all the patients included in the study were in critical condition when they were admitted. Increased levels
of troponin-T correlated with the severity of the condition; in deceased patients, the level of troponin was significantly higher
than in discharged patients. It should be noted that the level of troponin-T in patients with AMI and other diseases practically
did not differ. There are reports in the literature that some severe diseases lead to an increase in the level of cardiac troponin-T
in the blood. In the present study, an increase in cardiac troponin-T was detected mainly in patients with multiple organ failure.
According to the literature data, it is multi-organ failure that leads to a "non-coronarogenic" increase in cardiac troponins in the
blood: for example, Ammann P., Maggiorini M., 2003, studied the level of troponin-T in patients with sepsis without AMI. As a
result of this study, it was shown that an increase in troponin-T was significantly more often detected in patients with septic
shock, which is the cause of multiple organ failure, while the level of troponin-T directly correlated with the level of tumor
necrosis factor-α (TNF-α) and interleukin-6 (IL-6). The authors suggest using troponin-T as an additional factor in the
unfavorable course of the disease in patients with a septic condition.
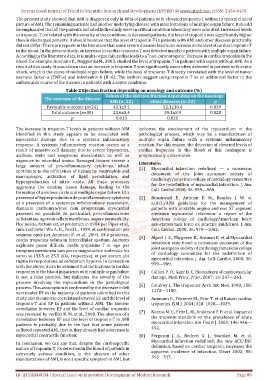
Table 2 Ejection fraction depending on nosology and outcome (%)
Values of the ejection fraction depending on the nosology
The outcome of the disease
AMI (n=22) other diseases (n=32) p
Favorable outcome (n=24) 43.1±9.1 52.1±10.4 0.039
Fatal outcome (n=30) 23.6±8.4 39.1±8.9 0.028
p 0.013 0.021
The increase in troponin-T levels in patients without AIM indicates the involvement of the myocardium in the
identified in this study appears to be associated with pathological process, which may be a manifestation of
myocardial damage due to a systemic inflammatory multiple organ failure with a systemic inflammatory
response. A systemic inflammatory reaction occurs as a reaction. For this reason, the detection of elevated levels of
result of massive cell damage due to severe hypoxemia, cardiac troponins in the blood of this contingent is
acidosis, endo and exogenous intoxication, as well as prognostically unfavorable.
exposure to microbial toxins. Damaged tissues secrete a
Literature:
large amount of pro-inflammatory cytokines, which [1]
contribute to the infiltration of tissues by neutrophils and Myocardial infarction redefined — a consensus
document of the Joint european society of
macrophages, activation of lipid peroxidation, and
cardiology/american college of cardiology committee
hyperproduction of nitric oxide. All these processes
for the redefinition of myocardial infarction. J. Am.
aggravate the existing tissue damage, leading to the Coll. Cardiol.2000; 36: 959—969.
formation of a vicious circle and multiple organ failure. Ut a
praecessi of hyperproduction de proinflammatory cytokines [2] Braunwald E., Antman E. M., Beasley J. W. et
ut a praecessi of a systemica inflammatione reactionem, al.ACC/AHA guidelines for the management of
damnum cardiomyocytes cum progressum myocardial patients with unstable angina and non ST segment
praesent est possibile. In particulari, pro-inflammatione elevation myocardial infarction: a report of the
substantiae, agere in cellam membrana, augere permeability. American college of cardiology/american heart
Hoc posito, factum est, et probatum in 1984 per Piper et al., association task force on practice guidelines. J. Am.
tunc sustinetur Wu A. H., Ford L., 1999, et confirmatum per Coll. Cardiol. 2000; 36: 970—1062.
sequens opus per Ammann P. et al., 2003. Ut a praecessi, [3] Alpert J. S., Thygesen K., Antman E. et al.Myocardial
cordis troponins soluta in intercellular spatium. Auctores
infarction rede fined: a consensus document of the
explicare posse diffusio cordis troponins-T et ego per
integrum membrana tam parva magnitudine moleculis his joint european society of cardiology/american college
of cardiology committee for the redefinition of
servo se (33.5 et 25.5 kDa, respective), et per eorum alia
myocardial infarction. J. Am. Coll. Cardiol. 2000; 36:
ruptio in responsione ad cellularum hypoxia. In connection
959—969.
with the above, it can be assumed that the increase in cardiac
troponins in the blood in patients with multiple organ failure [4] Collins P. O., Gaze D. C. Biomarkers of cardiovascular
is not a false positive, but indicates the severity of the damage. Med. Princ. Pract. 2007; 16: 247—261.
process involving the myocardium in the pathological [5]
process. This assumption is confirmed by the decrease in left Coudrey L. The troponins. Arch. Int. Med. 1998; 158:
1173—1180.
ventricular EF in the majority of patients identified in this
study and the inverse correlation between EF and the level of [6] Ammann P., Pfisterer M., Fehr T. et al.Raised cardiac
troponin-T and EF in patients without AMI. The inverse troponins. B.M.J. 2004; 328: 1028—1029.
correlation between EF and the level of cardiac troponins [7]
was revealed by verElst K. M. et al., 2000. The absence of a Kontos M. C., Fritz L. M., Anderson F. P. et al. Impact of
the troponin standard on the prevalence of acute
correlation between EF and the level of troponin-T in AMI
patients is probably due to the fact that some patients myocardial infarction. Am. Heart J. 2003; 146: 446—
452.
suffered repeated AMI, that is, they already had a decrease in
myocardial contractile function. [8] Ferguson J. L., Beckett G. J., Stoddart M. et al.
Myocardial infarction redefined: the new ACC/ESC
In conclusion, we can say that, despite the cardiospecific
nature of troponin-T, its detection in the blood of patients in definition, based on cardiac troponin, increases the
apparent incidence of infarction. Heart 2002; 88:
extremely serious condition, in the absence of other
343—347.
manifestations of AMI, is not a specific symptom of AMI, but
ID: IJTSRD40034 | Special Issue on Innovative Development of Modern Research Page 89